Thanks for subscribing!
You will now receive future content from Lyra Health.

COVID-19 has introduced a unique set of challenges for the American worker: From sudden and wide-reaching stay-at-home orders, to the obstacles of working remotely and an overwhelming feeling of doom, many employees are having trouble coping with day-to-day pandemic life. What used to be a beer at happy hour with coworkers has become four cocktails in the early afternoon for many; so to what extent, exactly, has the coronavirus pandemic impacted substance use disorders?
Long before the pandemic hit, news headlines flooded our country about the Opioid Overdose Epidemic. According to the Centers for Disease Control (CDC), this particular epidemic has been a problem since 1999, and over 450,000 people have died since then from overdoses. The rise has been particularly concerning over the last few years.
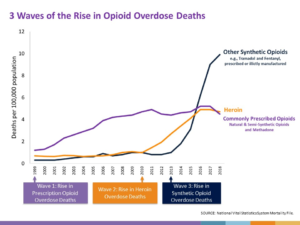
Opioid Overdose. Report by the CDC: https://www.cdc.gov/drugoverdose/epidemic/index.html
In addition to opioids, alcohol and tobacco continue to destroy Americans’ health. Tobacco and alcohol have represented the first and third leading preventable causes of death in the country, accounting for over half a million deaths annually.
These statistics on alcohol and tobacco illustrate the toll of these substances in the U.S.:
Having an alcohol use disorder or any substance use disorder is a clinical diagnosis and means that use has become so severe that it affects at least two dimensions of functioning. Meanwhile, the Substance Abuse and Mental Health Services Administration (SAMHSA) reports that people with substance use disorders have not been getting the treatment they need. While 8 percent of people report needing treatment for substance use disorders, only 1.5 percent actually receive it.
There was already a clearly trending crisis of substance use, substance use disorders, and access to treatment before 2020. Then, the pandemic hit.
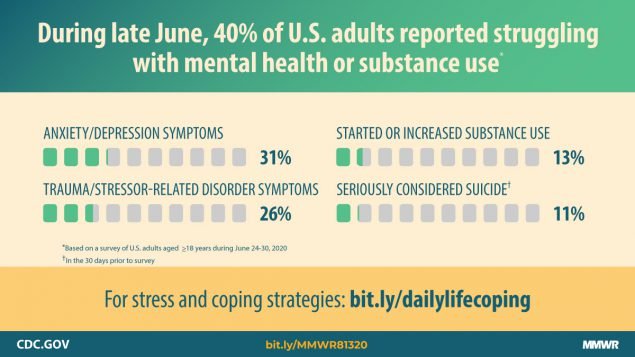
Mental Health, Substance Use, and Suicidal Ideation During the COVID-19 Pandemic — United States, June 24–30, 2020. Report by the CDC: https://www.cdc.gov/mmwr/volumes/69/wr/mm6932a1.ht
A pivotal report by the CDC this summer found that 13 percent of people started or increased their substance use this year. To make matters worse, almost 1 in 3 people have experienced anxiety or depressive symptoms, and over 40 states report a sharp rise in overdose deaths since the pandemic. Worse yet, people with substance use disorders are nearly 9 times as likely to contract COVID-19. And if they contract COVID-19, they’re more likely to have worse outcomes– for example, hospitalization and death. The story is even harsher for African Americans with substance use disorders: Their outcomes are disproportionately worse, pointing to another way in which COVID-19 has highlighted the already-concerning health disparities our nation faces.
Fortunately, we have evidence-based methods of approaching substance use disorders that have been proven to work. National guidelines recommend that we treat people in the least restrictive setting, and sooner rather than later. The earlier we can screen for and address substance use or risky substance use, the better outcomes are.
Furthermore, half of people with substance use disorders have another psychiatric diagnosis, like anxiety or depression. Treating both is paramount to the overall health and success of the individual.
With shelter-in-place precautions, we have seen a shift to virtual care and creative options for treatment. Even treatment that was formerly addressed in residential settings has shifted to virtual care, which may result in more sustainable treatment plans for individuals. Restrictions to access, reimbursement, and regulations have eased to make sure people can get care. On a larger scale, there is much-needed attention being paid to the pandemic’s impact on mental health.
Pre-pandemic, our nation made slow and steady progress to improve access to care for people with mental illness. Still, that progress has lagged with substance use disorders. Now, we are trying to catch up with the pandemic to provide care for a very deserving and vulnerable population: Federal and state regulations are more flexible with telemedicine restrictions and patients can now be reimbursed for more regular telemedicine visits. We applaud these policy changes; we also applaud advocacy, and benefit expansion to help those in need. We applaud the individual health care providers across multiple disciplines who have always treated people with substance use disorders using nonjudgmental, evidence-based methods. And finally, we applaud and have tremendous respect for the brave individuals suffering from substance use and substance use disorders who reach out for help.
A tremendous amount of work has been done to destigmatize mental illness and treatment. Substance use disorders are an equally important subset of mental illness that deserve the same nonjudgmental approach and de-stigmatization. As substance epidemics meet this evolving pandemic, we must rise to the occasion for the sake of our nation’s health.
CONTACT US
If you want help connecting with a therapist, Lyra can assist you. You can get started today if Lyra is offered by your employer. Sign up now.
For employers who want to learn more about how Lyra’s enhanced EAP addresses network adequacy and quality issues, download our whitepaper on quality or get in touch.
And check in frequently here or follow us on Facebook, LinkedIn, and Twitter for more insights into supporting employees’ mental health.
DISCLAIMER
The content of this blog is not intended to be a substitute for professional medical advice, diagnosis, or treatment.
ABOUT THE AUTHOR
Smita Das, MD, PhD, MPH is Medical Director of Psychiatry at Lyra Health. She is an addiction psychiatrist and public health researcher, serving as a leader in local and national committees in psychiatry. She also practices at Stanford University School of Medicine, where she is a clinical assistant professor.