Menopause and Mental Health: Promoting a Healthy Mindset
March 1, 2024
Women and people with ovaries typically begin to undergo the menopausal transition starting in their 40s. The transition starts with perimenopause, which is marked by increasingly irregular periods, and can last several months to a decade. The transition ends with postmenopause, or 12 months after the person’s last period.
The menopausal transition affects our bodies in profound ways that may feel intense and overwhelming at times.
How do I know if I’m experiencing menopause?
Commonly experienced symptoms include:
- Hot flashes
- Night sweats
- Sexual difficulties
- Weight change
- Aggravated existing health issues
- Headaches
- Brain fog
- Memory problems
- Trouble sleeping
- Irritability
- Increased sensitivity
- Mood swings
- Depression
- Anxiety
Menopause symptoms are unique to each person, with some individuals experiencing severe or prolonged symptoms. For help managing your symptoms, it’s important to discuss them with your medical and mental health providers. There are also things we can do on our own to support our mental health through the transition.
Challenging stigma and unhelpful beliefs
Harsh stigma around menopause and mental health can further complicate the experience. But uncomfortable subjects like menopause can be approached with greater ease when we consider them openly, better understand their influence on mental health, and use effective coping strategies to address menopause and depression or anxiety.
The first step is to recognize that menopause isn’t a disease or something to be ashamed of. Menopause is a natural part of life that presents both challenges and opportunities for personal growth. Talking to people you trust about your experience with menopause can help break down the stigma. Accepting menopause as a part of life can also decrease the distress of menopause and anxiety so that we can think about it in more helpful ways.
Menopause and mental health
It’s common to experience menopause and depression and menopause and anxiety, along with other mental health challenges, throughout the menopausal transition. According to The American College of Obstetricians and Gynecologists, roughly four in 10 women experience mood changes during perimenopause. Several other factors can affect our mental health during the menopausal transition, including:
- Hormonal changes
- Physical discomfort
- Changes in appearance
- Life pressures or changes (caregiving, kids leaving home, etc.)
- Grief over loss of youth, regret
- Negative thoughts about menopause and its symptoms
Why mindset matters
How we think about menopause and its symptoms typically affects how we feel—emotionally and physically. Thoughts that increase emotional distress can intensify physical symptoms.
How the Menopause Mindset Affects Us
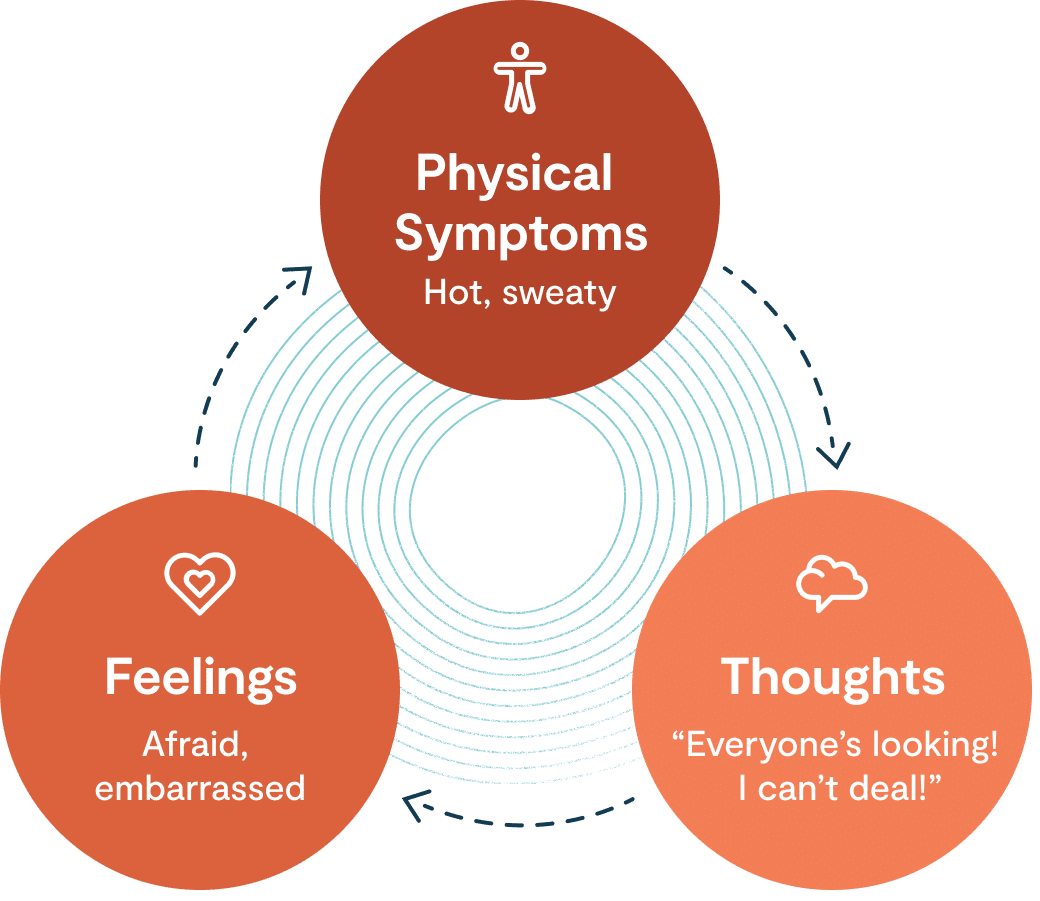
Negative beliefs about menopause and aging may be connected to depression. Similarly, worrisome thoughts about menopause symptoms or meeting life’s demands may contribute to the link between menopause and anxiety. While we can’t stop menopause, we can reshape our thinking to ease physical and emotional symptoms.
Challenging “thinking traps” for a healthy mindset
Thinking traps are automatic thoughts that can stimulate painful emotions. These thoughts are often rooted in assumptions that we tend to believe without questioning their accuracy. Noticing and questioning thinking traps can help us reevaluate our perception and experience with menopause. The following is a three-step process to help challenge thinking traps when they happen:
-
Recognize the thinking trap. When feeling down or distressed, ask yourself: “Is this a thinking trap?” Here are a few common ones:
-
Catastrophizing: Assuming menopause will have majorly detrimental effects and underestimating our capacity to cope.
Example: “This hot flash means something’s wrong with me! I can’t deal with it!” -
All-or-nothing: Viewing menopause and its symptoms as entirely bad.
Example: “Going through menopause is awful in every way.” -
Personalizing: Blaming ourselves for menopause symptoms.
Example: “I’m a terrible person for being so cranky.” -
Mind reading: Assuming we know what others think or feel about us.
Example: “People are judging me for sweating so much.” -
Overgeneralizations: Making broad assumptions about future experiences with menopause based on single events.
Example: “I can’t sleep! I’ll be exhausted for years to come!”
-
Catastrophizing: Assuming menopause will have majorly detrimental effects and underestimating our capacity to cope.
-
Question the thinking trap. Using a kind and curious tone, ask yourself:
- Am I overestimating the possibility of something bad happening?
- Am I underestimating my coping abilities?
- How have I managed similar situations?
- What would I say to a close friend who had this thought?
- What neutral or beneficial aspects might I be ignoring?
-
Generate more helpful thoughts. Considering your answers to the questions above, ask yourself, “What is a more helpful thought?” Think of as many alternatives as you can. More helpful thoughts might include:
- “I can cope with one hot flash or sleepless night at a time.”
- “I’m probably noticing my symptoms more than other people.”
- “This won’t last forever.”
- “These symptoms are natural. I’m OK.”
- “Aging isn’t all bad—I’m wiser!”
Offering yourself kindness
Spend a few moments to reflect on how you can best care for yourself, using the guidance below:
- Pause all other activities, and settle into a comfortable position.
- Notice your feet on the floor and the support of the surface beneath you, and take some slow breaths.
- Ask yourself: “What do I really need right now?” Be open to the answer.
- Next, ask yourself: “What can I do to show myself kindness in this moment?” Listen to the answer, and do your best to offer yourself care.
Lyra is here for you
For more help navigating menopause and mental health challenges, book a session with our mental health experts.
Author
The Lyra Team
The Lyra Team is made up of clinicians, writers, and experts who are passionate about mental health and workplace well-being. With backgrounds in clinical psychology, journalism, content strategy, and product marketing, we create research-backed content to help individuals and organizations improve workforce mental health.
Explore additional blogs

Mental health tips
How Radical Acceptance Can Decrease Your Stress

Mental health tips
Empty Nest Syndrome: Missing Them, Finding You

Mental health tips